What is lung cancer?
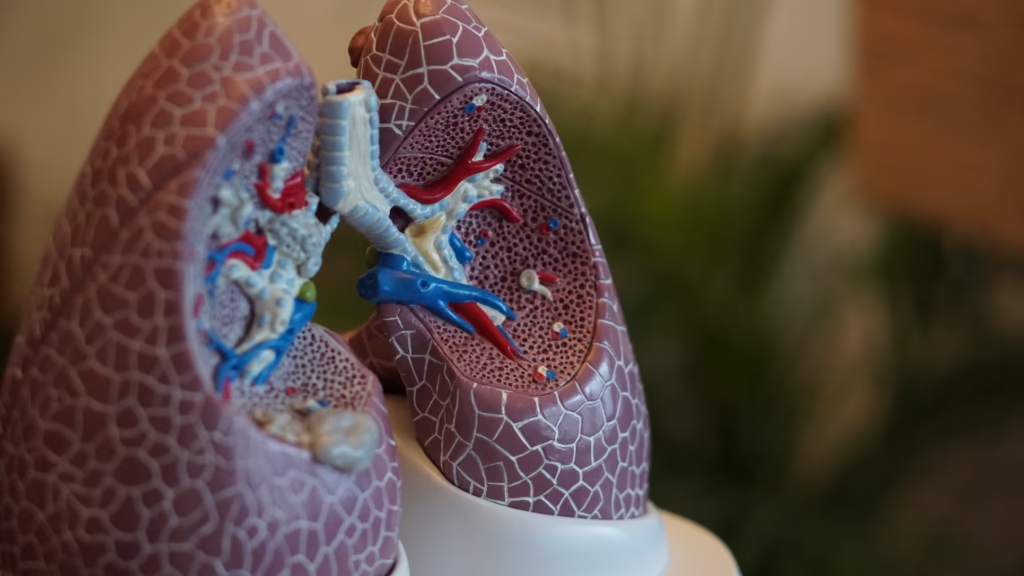
Lung cancer is a malignant growth that originates in the lung tissues when normal lung cells change to abnormal cells, which multiply uncontrollably and invade the surrounding healthy lung tissues. The cancerous cells can spread to other parts of the body via lymphatic or blood vessels by a process known as metastasis.
According to Global Cancer Observatory (GLOBOCON) 2020 cancer statistics and estimates of 36 cancers from 186 countries, lung cancer is the second most common cancer worldwide, surpassed only by breast cancer.It causes the highest number of cancer deaths, about 1.8 million deaths annually.
What are the risk factors for lung cancer?
The following are risk factors for lung cancer:
Cigarette smoking
Cigarette smoking is the most significant factor in developing lung cancer. The likelihood of lung cancer increases with the amount of cigarettes smoked and the number of years of being a smoker. This occurrence could be attributed to damage to the cells that line the lung surface (epithelial cells) because of long-term exposure to cigarette smoke. Epithelial cell damage results in abnormal cell formation (dysplasia) and alteration of a series of events involved in cell growth and division (cell cycle), which might eventually lead to cancer growth (carcinogenesis).
Second hand or passive smoking
Second hand or passive smoking also contributes to the development of lung cancer. Involuntary inhalation of smoke from tobacco products used by others (passive smoke) raises the risk of lung cancer among non-smokers. Second hand smoke contains polycyclic aromatic hydrocarbons and other harmful substances that cause lung cancer. Continuous exposure to passive smoke for more than 20 years significantly increases the likelihood of lung cancer, especially among women.
Asbestos
Exposure to asbestos, a naturally occurring fibrous substance, in occupational settings such as mining, construction and ship building has contributed to lung cancer risks and deaths. Inhaled asbestos fibres can cause direct damage to lung epithelial cells, resulting in inflammation, cellular injury, and eventually carcer.
Radon
Radon, a natural radioactive gas, can accumulate in homes, especially basements and poorly ventilated areas. It has been identified as a risk factor for lung cancer. Research conducted among uranium miners, often exposed to high levels of radon, showed a remarkable association between cumulative radon exposure and lung cancer, supporting the view that radon is a potent cancer-causing substance (carcinogen)
Nickel
Exposure to nickel dusts or fumes in industries causes lung cellular damage, leading to genetic alteration (mutation) and cancer development.
Chronic lung disease, e.g. Chronic Obstructive Pulmonary Disease
Patients with chronic lung diseases such as chronic obstructive pulmonary disease (COPD) have a higher likelihood of lung cancer than those without chronic lung diseases.
COPD often causes ongoing inflammation in airways and lung tissue, which can damage cells and promote cancer growth.
Genetic factors and family history
Genetic factors and family history also play a role in the development of lung cancer, particularly in non-smokers. This predisposition is significant in individuals that harbour a genetic abnormality in a molecule known as epidermal growth factor receptor (EGFR)
What are the symptoms and signs of lung cancer?
The following features are suggestive of lung cancer:
- Persistent cough up to 3 weeks
- Coughing up of blood (haemoptysis)
- Shortness of breath
- Chest pain
- Weight loss
- Loss of appetite
- Unexplained tiredness
- Facial and neck swelling
Some of the symptoms of lung cancer are not specific to it; as such, they may be seen in other cancers or chronic diseases. In many cases, patients do not present until the disease has advanced because they might not attribute their symptoms to lung cancer. If you or someone you know has the symptoms listed above, go to your doctor for an assessment. Early detection of lung cancer is important for a better outcome.
How can lung cancer be diagnosed?
Diagnosis of lung cancer starts with suspicion of signs and symptoms. Patients require imaging of the lung and biopsy, which entails tissue sampling from the lungs for microscopic examination and diagnosis.
In collecting lung biopsy, doctors favour minimally invasive methods that take tissue samples from the most accessible locations in the lung for the sake of patient safety, minimising complications and having enough tissue to establish a diagnosis (diagnostic yield).
For patients who have a centrally located tumour, a bronchoscope—a hollow instrument with a camera attached—is used to view the airway and area of tumour. A biopsy is then taken from the tumour site for tissue diagnosis.
When patients have a centrally located lung tumour but are not fit for bronchoscopy, sputum examination for cancer cells (sputum cytology) is done, especially to detect early-stage lung cancer.
For patients with peripherally located tumours, a biopsy is taken by insertion of a needle through the skin surface to obtain a sample from the tumour (percutaneous biopsy). The technique is particularly beneficial for peripheral lesions since it is minimally invasive and has the capacity to correctly target the tumour utilising imaging guidance, such as ultrasound or computed tomography.
In some instances, diagnosis of lung cancer may be made without tissue diagnosis if patients meet the criteria.
What are the types of lung cancer?
There are two main types of lung cancer based on appearance under the microscope (histologic examination) and the mode of management
1. Small cell lung carcinoma (SCLC): when examined under a microscope, SCLC is characterised by small, oval cells that exhibit scant cytoplasm and a high nuclear-to-cytoplasmic ratio.
The tumour grows in large airways in the centre of the chest and is often associated with cigarette smoking. Patients frequently present with advanced disease, defined by the existence of metastases beyond the primary tumour
2. Non-small cell carcinoma (NSCC): they are the most common type of lung cancer. They are classified into the following sub-types:
a. Adenocarcinoma: histologically, the tumour is made up of abnormal glands or ducts. The tumour commonly grows in the periphery of the lung tissue.
The prevalence of lung adenocarcinoma is increasing, particularly among nonsmokers and younger populations, which is due in part to the rising prevalence of specific genetic abnormalities, such as those in the epidermal growth factor receptor (EGFR) gene.
Most patients are diagnosed at an advanced stage, which negatively impacts the disease prognosis.
b. Squamous cell carcinoma: when examined under a microscope, it is often characterised by the presence of keratin and intercellular bridges. The tumour originates from squamous epithelial cells that line the airways and grow in the upper part of the lung tissue close to the hilum. It is associated with smoking.
c. Large Cell Carcinoma (LCC): histologically, large cell carcinoma is characterised by the presence of large, polygonal cells with abundant cytoplasm and prominent nucleoli. The tumour grows either centrally or peripherally in lung tissue.
The main risk factor for LCC is tobacco smoking.
What are the treatment options for lung cancer?
Treatment for lung cancer depends on the type and stage of lung cancer as well as the general health of the individual.
The treatment options include:
1. Surgery: Surgery is frequently the first-line treatment for early-stage lung cancer, especially non-small cell lung cancer (NSCLC). The surgical options are lobectomy (removal of a lobe of the lung), pneumonectomy (removal of the entire lung), and wedge resection (removal of a small, triangle-shaped piece of lung tissue containing tumour and some surrounding healthy tissue).
The purpose of surgery is to remove the tumour and any surrounding tissue that may contain cancer cells.
2. Chemotherapy: chemotherapeutic drugs are used to kill cancer cells or stop them from growing. They are commonly used for both NSCLC and small cell lung cancer (SCLC), particularly in cases where the cancer has spread beyond the lungs.
Chemotherapy can be used as a palliative medicine, neoadjuvant (before surgery) therapy, or adjuvant (after surgery) therapy. While it can be effective in reducing tumour size and controlling symptoms, it is associated with significant side effects, including nausea, fatigue, and increased risk of infection.
3. Radiation therapy: often used in conjunction with surgery and chemotherapy. It can be employed as a curative treatment for localised tumours or as palliative care to relieve symptoms in advanced cases. Radiation therapy works by damaging the DNA of cancer cells, preventing them from dividing and growing.
4. Targeted therapies: Specific genetic mutations, e.g., epidermal growth factor receptor (EGFR), can be targeted in the treatment of lung cancer. Drugs such as erlotinib and gefitinib target the epidermal growth factor receptor (EGFR), which is often mutated in lung adenocarcinoma.
Support and Resources
Check out the following link for support and resources on lung cancer: